Strain vs Sprain
STRAINS
s"T"rain = "T"endon
Overstretch injury to musculotendinous unit (tendon)
Concentric: Mxl contraction as the origin and insertion of the mxl comes closer together, Mxl fibres shorten
Eccentric:Origin and insertion move farther apart, the mxl fibres lengthen
Eccentric contraction can produce. greater force within the mxl than concentric contraction, predisposing the mxl to injury at this time
Hypovascular nature of tendons contributes to decreased tissue health, allowing the tendon itself to rupture
Fun fact!
The younger people where the epiphyseal plate in the bone has not yet ossified, the mxl and tendons are stronger than the bone!
Because tendons are moderately vascularized, they are prone to partial or complete rupture at the area of least blood supply either in the middle of the tendon or at the musculotendinous junction.
Concentric: Mxl contraction as the origin and insertion of the mxl comes closer together, Mxl fibres shorten
Eccentric:Origin and insertion move farther apart, the mxl fibres lengthen
Eccentric contraction can produce. greater force within the mxl than concentric contraction, predisposing the mxl to injury at this time
Hypovascular nature of tendons contributes to decreased tissue health, allowing the tendon itself to rupture
Fun fact!
The younger people where the epiphyseal plate in the bone has not yet ossified, the mxl and tendons are stronger than the bone!
Because tendons are moderately vascularized, they are prone to partial or complete rupture at the area of least blood supply either in the middle of the tendon or at the musculotendinous junction.
What is the cause of STRAINS?
Sudden overstitching of the mxl
Extreme contraction of the mxl against heavy resistance
3 grades of Severity
Grade 1: Mild
Minor stretch and/or tear
Minimal loss of strength
Grade 2: Moderate
Tearing of musculotendinous fibres
There may be snapping sensation or sound at time off injury
Unable to continue activity d/t mxl weakness and pain
Grade 3: Severe
Complete rupture of the musculotehdinous unit or an avulsion fracture as the body attachment of the tendon is torn off while the unite remains intact
Palpable/visible gap appears at the injury site
Often mxl shortens and bunches up
Unable to continue activity d/t signifiant pain and mxl weakness
SXS
Acute:
Grade1: Local edema, heat, bruising
tenderness at site of injury
Little to no loss of strength or ROM
Capable of continuing the activity
Grade2: Tearing of several or many fibres of the musculotendinous unit
Snapping noise or sensation at the site
Gap may be palpable
Moderate tenderness
Moderate pain with activities that contrast or stretch the musculotendinous unit
Moderate loss of strength and ROM
Hematoma on site
Bruising: Red, black, blue
Grade3: Complete rupture
Snapping noise or sensation at the time or injury
Local edema
Gap palpated in the tissue
Mxl will likely bunch up d/t spasmodic contractions
Severe pain
Immediate loss of strength and ROM
Unable to continue activity
Bruising: Red, black, blue
Hematoma on site
Ruptured mxl in lower limbs is usually surgically repaired and then immobilized in a cast for 4-8wks
Snapping noise or sensation at the time or injury
Local edema
Gap palpated in the tissue
Mxl will likely bunch up d/t spasmodic contractions
Severe pain
Immediate loss of strength and ROM
Unable to continue activity
Bruising: Red, black, blue
Hematoma on site
Ruptured mxl in lower limbs is usually surgically repaired and then immobilized in a cast for 4-8wks
Early subacute:
Grade1: Little to no pain and reduced strength
Grade2: Pain and moderately reduced strength
Grade3: Pain and markedly reduced strength w/ARROM
Pain, edema and inflammation are still present
Adhesions are developing around the site of injury
b/o poor vasculature, healing is relatively slow
Mxl guarding spasm diminishes
TrP occurs in the affected mxl, its synergist and its antagonists
Reduced ROM
Grade1: Little to no pain and reduced strength
Grade2: Pain and moderately reduced strength
Grade3: Pain and markedly reduced strength w/ARROM
Pain, edema and inflammation are still present
Adhesions are developing around the site of injury
b/o poor vasculature, healing is relatively slow
Mxl guarding spasm diminishes
TrP occurs in the affected mxl, its synergist and its antagonists
Reduced ROM
Late subacute:
Bruising: Yellow, Green, Brown
Hematoma diminishes
Gap is still palpable
Protective mxl spasm is replaced by increased tone in the affected mxl, its synergists and its antagonists.TrP occur in affected mxl and in compensatory mxl
Adhesions are maturing around the injury
Reduced ROM
Chronic:
No more bruising
Hypertonicity and TrP are present
Adhesions have matured around the injury
Tissue may be cool d/t ischemia
Full ROM of the joint may be reduced with Grade 2 & 3
Repetitive injury from overuse is too stressful for the mxl
Pocket of chronic edema may remain local to the site
Reduced strength of the affected musculotendinous unit and possible disuse atrophy may present
No more bruising
Hypertonicity and TrP are present
Adhesions have matured around the injury
Tissue may be cool d/t ischemia
Full ROM of the joint may be reduced with Grade 2 & 3
Repetitive injury from overuse is too stressful for the mxl
Pocket of chronic edema may remain local to the site
Reduced strength of the affected musculotendinous unit and possible disuse atrophy may present
Questions to ask
Health Hx
Rx
Hx of strain (Is this the first time to strain? You have had it before at the same site?)
Did you hear any popping sound when you injured?
Were you assessed by MD?
Do you see anybody else? Chiro, Physio, etc.
Any hematoma, nerve damage or avulsion at the tendon's attachment?
What are you currently feeling?
Palliative & provocative
Swelling on site or distal to the site of injury?
With strain of wt bearing limb, did the limb "Give way" at the time of injury? >>> Indication of Grade 3 strain
Observation
Acute: Gait analysis
Taping or bandages or splint
Edema
Some redness
Early and late subacute:
Bruising
Early subacute-Purple and black
Late subacute-Yellow and green
Chronic:Habituated gait and posture may be observed w/ strain
Visible gap at the lesion site might be present from grade 3 strain
Scar might be formed if musculotendinous unit is reduced surgically
Palpation
Acute
Heat and tenderness present
Firm edema
Palpable gap
Protective mxl spasm
Mxl guarding
Early and Late subacute
Temperature on the site is diminishing
Local tenderness may present
Palpable gap or alteration in the Mxl's contour and hypertonicity
TrP in affected Mxl
Chronic
Cool to touch d/t ischemia
Tenderness to the lesion site
If it is on shoulder, they may not be able to sleep on affected side
Palpable gap may present w/ Grade 2 & 3
Hypertonicity and TrP may be present
Disuse atrophy in affected mxl
Testing
Acute: ARROM of affected mxl is reduced
Other testing is CONTRAINDICATED in acute stage if Grade2&3 are suspected
How can you tell?
Acute
Snapping sensation at the time of injury?
Difficulty continuing the activity or unable to continue ADL?
Palpa ble gap?
ARROM?
Early and Late Subacute
AROM?
ARROM?
AR isometric contraction?
Grade1: minor loss of strength, minor pain
Grade2: Moderate loss of strength, Pain
Grade3: Significant loss of strength, Pain
Chronic
AROM:May be limited
ARROM
Mxl strength testing: Decreased w/disuse atrophy or Grade 3 strains
Special test for Strain
Thompson's test
Yergason's test(if strain is in the shoulder)
Drop arm test (if strain is in the shoulder)
Aply's scratch test
Thomas and Ely's test
Mxl length test of injured site
Treatment plan
Acute: Mxl is treated with RICE
Positioning: elevate affected area with pillow
Hydrotherapy: Cold
Hydrotherapy: Cold
Early & Late Subacute
Stroking and squeezing tech distal to the site of injury
Hydrotherapy: Cold/Warm contrast
Stroking and squeezing tech distal to the site of injury
Hydrotherapy: Cold/Warm contrast
TrP
Promote ROM
Lymphatic drainage
Chronic
Outcomes
Acute: Reduce inflammation & edema
Reduce pain
NO direct tx on site
Early & Late subacute: Reduce inflammation & edema
Mid range PROM
Reduce spasm
TrP
Reduce adhesion
Chronic: Reduce sympathetic nervous sys tem firing
Reduce any chronic edema
TrP
Decrease tone
Restore ROM
Promote blood circulation to the injured site
Treat scar if mxl was surgically repaired Self Care
Hydrotherapy
Self massage
Maintain strength of the affected mxl in the pain-free manner
Stretch shortened mxl
Increase strength gradually
Encourage activity
Frequency
Acute: Shorter more frequent tx
Chronic: Longer, weekly tx
Grade1:Possible to return to activity with a support after 2 days
Grade2:Possible to return to activity after several days to several weeks
Grade3:Immobilization could be removed after 4-8 weeks
Return to activity after 8 weeks but may delay for up to several weeks d/t atrophy of the mxl
SPRAINS
Overstretch injury to a ligament
They can still continue some activities with some discomfort
Grade2-Moderate:Tearing of Lig. fibres occurs
Snapping sound at the time of injury and Jt. gives way
Hyermobile yet stable on passive relaxed testing
They may have difficulty continuing the activity
Grade3-Severe:Complete rupture of the Lig. itself or avulsion fracture as the body attachment of the Lig. is turnoff while the Lig. remains intact
Surgically repaired or treated by the medically conservative approach of immobilization of the Jt. in a cast or strapping
Common sprains
Lateral ankle Lig.
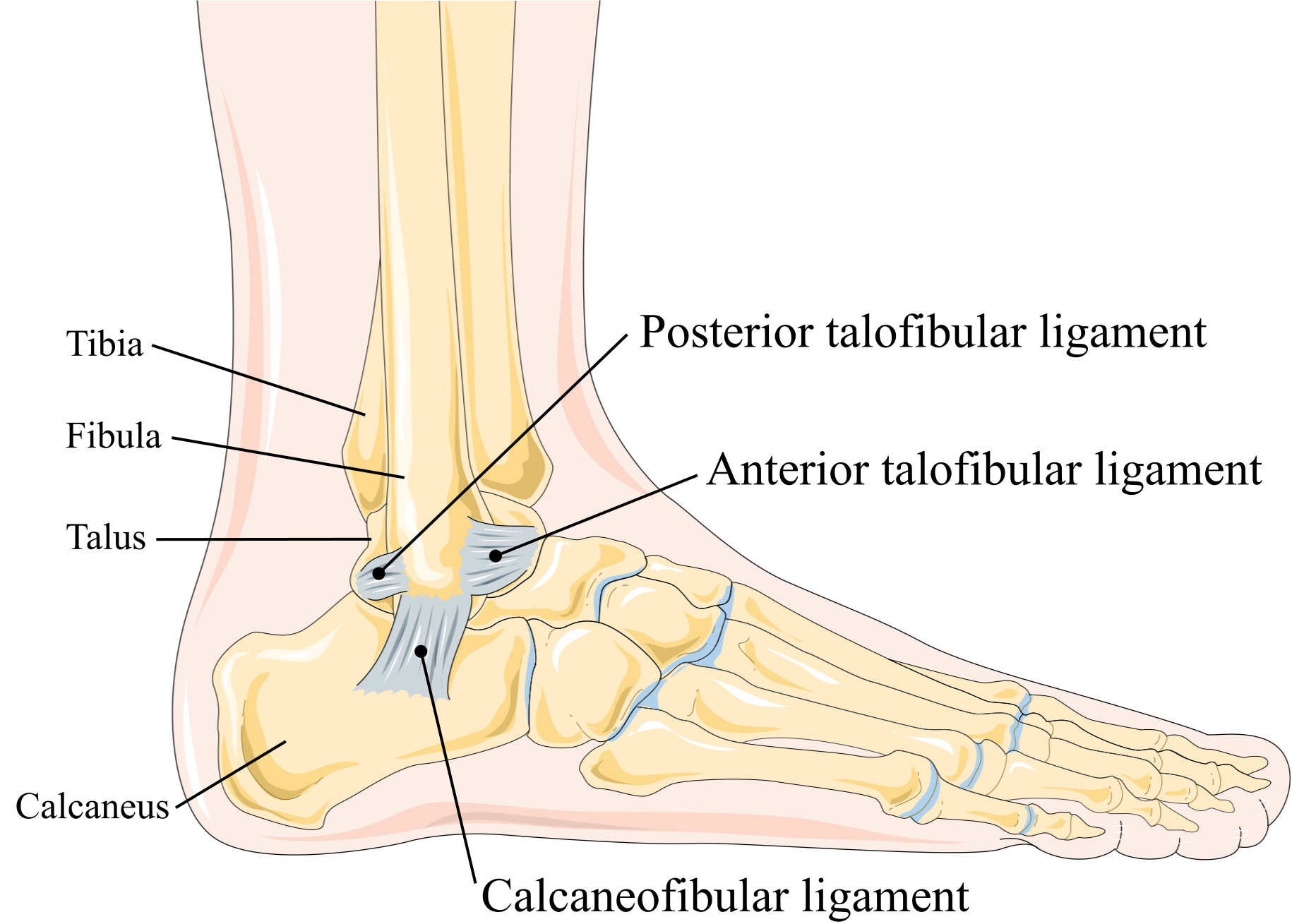
MC Lig. of sprain (Inversion sprain) are
Ant. talofibular Lig.
Post. talofibular Lig.
Calcaneofigular Lig.
 MC Lig. of sprain
MC Lig. of sprain

Grade1:Minor stretch to Lig
Mild pain, minimal edema, stable Jt
May continue activity
Grade2:Tearing of some or many fibres of the Lig
Snapping noise and Jt gives way
Moderate pain, edema, heat and bruising are present
Slight Jt instability
May have difficulty continuing the activity d/t pain
Grade3:Complete rupture or Avulsion Fx of Lig attachment
Snapping noise, Intense pain, significant edema, heat, bruising
Hematoma, Jt effusion may be present
Jt instability
Unable to continue activity
Early subacute
Grade1:Stable
Grade2:Hypermobile yet stable
Grade3:Hypermobile and unstable w/Liamentous stress testing
Bruising: Black and blue
Pain, edema inflammation are still present but reduced
Adhesions are developing around the injury
d/t hypo vascular characteristic, it heals relatively slow
When protective spasm diminishes, TrP occurs on the site of injury and compensatory mxl
Reduced ROM
Loss of Proprioception at the Jt
Late subacute
Bruising: Yellow, green brown
Pain, edema, inflammation are diminishing
Adhesions are maturing around the injury
Increased tone of mxl crossing the Jt
Affected Jt may still be supported
Reduced ROM
Loss of proprioception at the Jt
Proprioception (or kinesthesia) is the sense though which we perceive the position and movement of our body, including our sense of equilibrium and balance, senses that depend on the notion of force (Jones, 2000)
Chronic
Pain local to the area only if the Lig is stretched
Bruising is gone
Adhesions have matured around the injury
Hyper tonicity and TrP are present
Full ROM of the Jt is restricted
Pocket of Chronic edema may remain local to the Lig
Mxl weakness or disuse atrophy may be present
They may still need some taping to support the Jt
Any pathology?
Did you hear any snapping sound at the time of injury?
Nerve damage?
Fracture?
Palliative/Provocative
Edema present at the affected Jt
If its Grade3, there may be distal edema present
Early and late subacute
Antalgic gait still present if sprain is in a Wt.bearing Jt
Chronic
Habituated antalgic gait and posture may be observed w/sprain or Wt. bearing Jt
Check Postural assessment!
There may be some edema local to the Lig. usually repetitive sprains of the same Jt
Tenderness to the lesion site
Edema is firm
Protective Mxl spasm
Early and late subacute: Heat diminishes as time goes
Tenderness to the lesion site
Edema is less firm and adhesions are resent as healing process from the early to late subacute
Mxl tone becomes tighter and high in late subacute
TrP are present in these Mxl
Chronic
Cool to touch d/t ischemia
Point tenderness occurs locally
Chronic edema:Boggy, jelly-like feeling
Adhesions local to the Lig
Crepitus may present
Hyper tonicity and TrP are local to the site of injury
Reduced ROM
Special test: Ballottable patella, Minor effusion test
Early and late subacute:
ROM, RROM
Isometric testing: Mxl crossing the affected jt are strong and painless w/strictly ligamentous injury. If mxl or tendons are also involved, there is pain at the lesion site in the contractile tissue
Special test: Ligamentous stress test, Ant drawer test (Ankle), Valgus or Varus, apple's distraction test, Brush test (Knee),
Chronic:ROM, RROM
Special test: Ligamentous stress test
Elevate the injured site
Cold hydrotherapy
Reduce pain and edema
Maintain local circulation proximal to the injury ONLY
Maintain ROM w/ mid range PROM
Early and late subacute
Reduce inflammation, Edema
Prevent from excess adhesion formation
Increase drainage and venous return w/ effleurage, petrissage (Palm kneading, c-scooping, fingertip kneading, ONI tech)
GTO is als used to that jt
Reduce TrP
Mid-range PROM to maintain ROM
Hydrotherapy: Hot/Cold
How do you reduce adhesions?
Short cross-fibre strokes and frictions to the ligament
Chronic
Hydrotherapy:contrast
PROM
Reduce adhesion: Cross fibre, Joint play(gentle)
Friction tech if they are taking anti-inflammatory or blood thinner
Self massage
Isometric contraction to strengthen the mxl
ROM to maintain Jt integrity
Chronic: Long duration & weekly tx
When can they return to their activity?Grade1: 4-5 days
Grade2:7-14 days
Grade3:6-8 weeks
However...
sprained Lig may take up to 6 months for full maturation of the collagen fibres
It is recommended to receive massage therapy for weekly or biweekly up to 6 months.
Trauma related sudden twist or wrench of the joint beyond its normal ROM
Cause
Congenital ligamentous laxity (Hypermobility)
Hx of previous sprains to that joint
Connective tissue pathology such as RA
Grade1-Mild: Minor stretch and tear to the ligamentThey can still continue some activities with some discomfort
Grade2-Moderate:Tearing of Lig. fibres occurs
Snapping sound at the time of injury and Jt. gives way
Hyermobile yet stable on passive relaxed testing
They may have difficulty continuing the activity
Grade3-Severe:Complete rupture of the Lig. itself or avulsion fracture as the body attachment of the Lig. is turnoff while the Lig. remains intact
Surgically repaired or treated by the medically conservative approach of immobilization of the Jt. in a cast or strapping
Common sprains
Lateral ankle Lig.
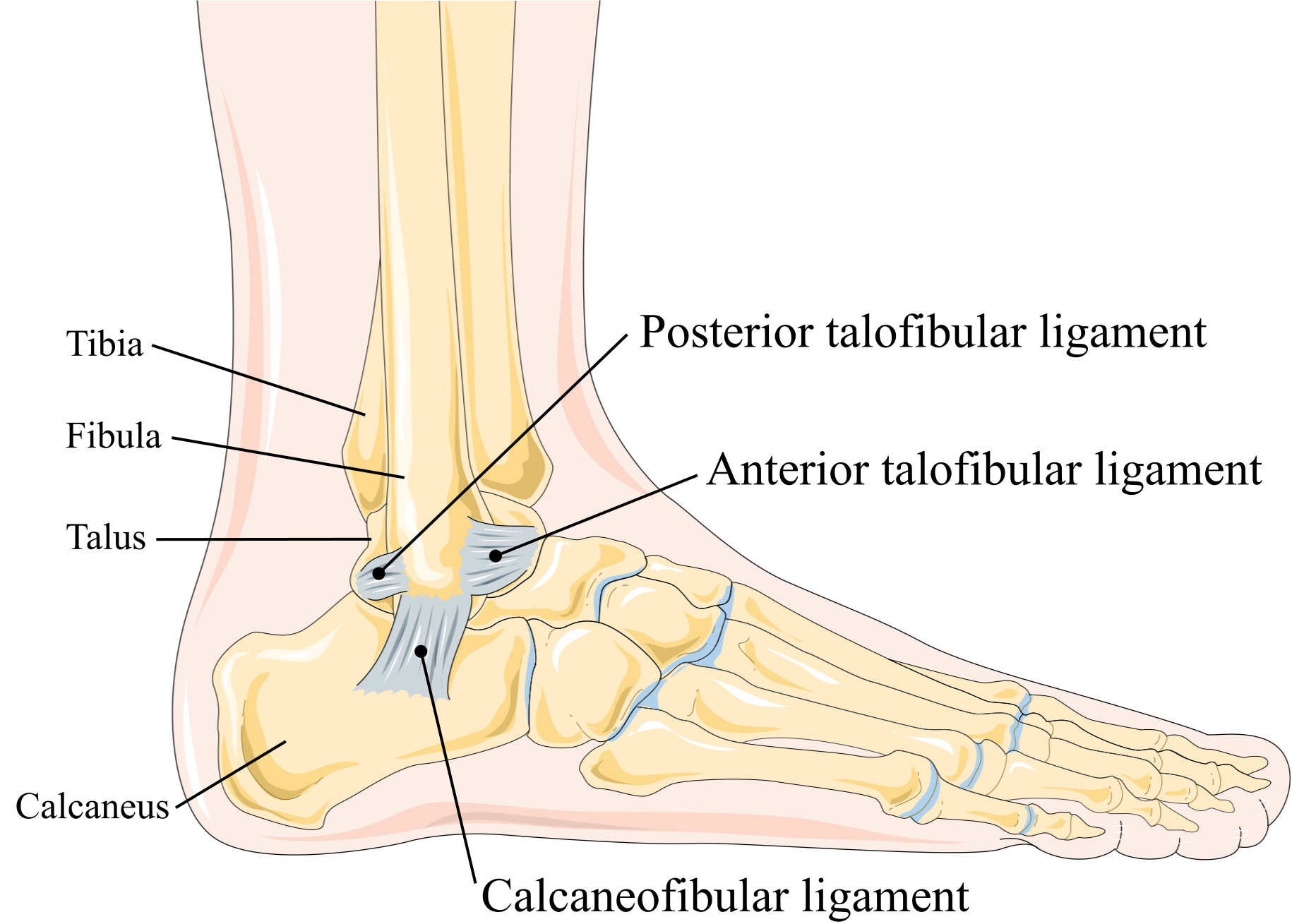
MC Lig. of sprain (Inversion sprain) are
Ant. talofibular Lig.
Post. talofibular Lig.
Calcaneofigular Lig.
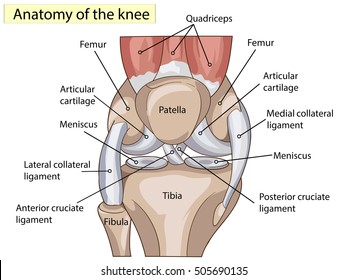
Knee Lig.
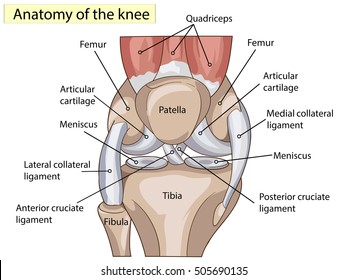
MCL, LCL, ACL, PCL,
Wrist Lig.
MC Lig. to be injured is Scapholunate ligament
Hyperextension of the wrist is usually the cause of the wrist sprain
Shoulder Lig.

Grade1: Acromioclaviular sprain involves tearing of Jt capsule
Grade2:Tear of the Jt capsule and acromioclavidular Lig
Grade3:Tear of the Jt capsule:Acromioclavidular Lig and conoid and
trapezoid Lig
Fx may also be present
SXS
AcuteGrade1:Minor stretch to Lig
Mild pain, minimal edema, stable Jt
May continue activity
Grade2:Tearing of some or many fibres of the Lig
Snapping noise and Jt gives way
Moderate pain, edema, heat and bruising are present
Slight Jt instability
May have difficulty continuing the activity d/t pain
Grade3:Complete rupture or Avulsion Fx of Lig attachment
Snapping noise, Intense pain, significant edema, heat, bruising
Hematoma, Jt effusion may be present
Jt instability
Unable to continue activity
Early subacute
Grade1:Stable
Grade2:Hypermobile yet stable
Grade3:Hypermobile and unstable w/Liamentous stress testing
Bruising: Black and blue
Pain, edema inflammation are still present but reduced
Adhesions are developing around the injury
d/t hypo vascular characteristic, it heals relatively slow
When protective spasm diminishes, TrP occurs on the site of injury and compensatory mxl
Reduced ROM
Loss of Proprioception at the Jt
Late subacute
Bruising: Yellow, green brown
Pain, edema, inflammation are diminishing
Adhesions are maturing around the injury
Increased tone of mxl crossing the Jt
Affected Jt may still be supported
Reduced ROM
Loss of proprioception at the Jt
Proprioception (or kinesthesia) is the sense though which we perceive the position and movement of our body, including our sense of equilibrium and balance, senses that depend on the notion of force (Jones, 2000)
Chronic
Pain local to the area only if the Lig is stretched
Bruising is gone
Adhesions have matured around the injury
Hyper tonicity and TrP are present
Full ROM of the Jt is restricted
Pocket of Chronic edema may remain local to the Lig
Mxl weakness or disuse atrophy may be present
They may still need some taping to support the Jt
Questions to ask
Health HxAny pathology?
Did you hear any snapping sound at the time of injury?
Nerve damage?
Fracture?
Palliative/Provocative
Observation
Acute: Antalgic gait if sprain is in a Wt.bearing JtEdema present at the affected Jt
If its Grade3, there may be distal edema present
Early and late subacute
Antalgic gait still present if sprain is in a Wt.bearing Jt
Edema diminishes both on site and distally
Bruising: changes from Purple and black to brown, yellow and green then disappears
If surgically reduced, scars are present
Habituated antalgic gait and posture may be observed w/sprain or Wt. bearing Jt
Check Postural assessment!
There may be some edema local to the Lig. usually repetitive sprains of the same Jt
If surgically reduced, scars are present
Palpation
Acute: Hot to touchTenderness to the lesion site
Edema is firm
Protective Mxl spasm
Early and late subacute: Heat diminishes as time goes
Tenderness to the lesion site
Edema is less firm and adhesions are resent as healing process from the early to late subacute
Mxl tone becomes tighter and high in late subacute
TrP are present in these Mxl
Chronic
Cool to touch d/t ischemia
Point tenderness occurs locally
Chronic edema:Boggy, jelly-like feeling
Adhesions local to the Lig
Crepitus may present
Hyper tonicity and TrP are local to the site of injury
Reduced ROM
Testing
Acute: ROM of proximal affected and distal jtSpecial test: Ballottable patella, Minor effusion test
Early and late subacute:
ROM, RROM
Isometric testing: Mxl crossing the affected jt are strong and painless w/strictly ligamentous injury. If mxl or tendons are also involved, there is pain at the lesion site in the contractile tissue
Special test: Ligamentous stress test, Ant drawer test (Ankle), Valgus or Varus, apple's distraction test, Brush test (Knee),
Chronic:ROM, RROM
Special test: Ligamentous stress test
Treatment Plan
Acute:RICEElevate the injured site
Cold hydrotherapy
Reduce pain and edema
Maintain local circulation proximal to the injury ONLY
Maintain ROM w/ mid range PROM
Early and late subacute
Reduce inflammation, Edema
Prevent from excess adhesion formation
Increase drainage and venous return w/ effleurage, petrissage (Palm kneading, c-scooping, fingertip kneading, ONI tech)
GTO is als used to that jt
Reduce TrP
Mid-range PROM to maintain ROM
Hydrotherapy: Hot/Cold
How do you reduce adhesions?
Short cross-fibre strokes and frictions to the ligament
Chronic
Hydrotherapy:contrast
PROM
Reduce adhesion: Cross fibre, Joint play(gentle)
Contraindications
Distal circulation techniques in acute and early subacute stage because this could increase congestion through the injury siteFriction tech if they are taking anti-inflammatory or blood thinner
Self care for all phase of healing
HydrotherapySelf massage
Isometric contraction to strengthen the mxl
ROM to maintain Jt integrity
Treatment frequency
Acute: Short duration & frequent txChronic: Long duration & weekly tx
When can they return to their activity?Grade1: 4-5 days
Grade2:7-14 days
Grade3:6-8 weeks
However...
sprained Lig may take up to 6 months for full maturation of the collagen fibres
It is recommended to receive massage therapy for weekly or biweekly up to 6 months.

Comments
Post a Comment