Collagen based tissue that develops as a result of the inflammatory process
Cause of scar tissue
Inflammatory response from wounds, burns, MSK trauma, inflammatory arthritis or late stage of osteoarthritis
Prolonged immobilization of a structure
Paralysis or paresis of a structure d/t peripheral or CNS lesion
Paresis: a condition of muscular weakness caused by nerve damage or disease
Type of scar
1.Contracture
This is different from the Muscle contracture!
It is a shortening of connective tissue supporting structures over or around the joint including mxl, soft tissue (tendons, joint capsules)
Soft tissue contractors include adhesions and irreversible contractures.


2.Adhesion
This occurs when reduced ROM allows cross-link to form among the collagen fibres, further reducing ROM.
MC when tissue left in a shortened position for prolonged period of time as in postural dysFCN or immobilization of a limb.


3.Scar tissue adhesion
This occurs with an injury or an acute inflammatory process. Collagen fibre formation during the tissue repair process allows adhesions and contractures to form a random pattern within skin, mxl, tendon, group of mxl and joint capsules. Adhesion also occurs within the joint
Usually can be treated with fascial tech, cross-fibre frictions, joint play, stretching
4.Fibrotic adhesion
Ongoing chronic inflammation can cause moderate to severe restrictions in ROM. Such adhesions are difficult to eradicate...


5.Irreversible contracture
When fibrotic tissue or bone replaces mxl and connective tissue. There is a permanent loss of ROM that can only be restored by surgical means..

When fibrotic tissue or bone replaces mxl and connective tissue. There is a permanent loss of ROM that can only be restored by surgical means..

6.Proud flesh
Thick dermal granulation tissue that results from an abnormal healing process.
Doctor could surgically cut back to the epithelial tissue level to reduce this type of scar tissues.
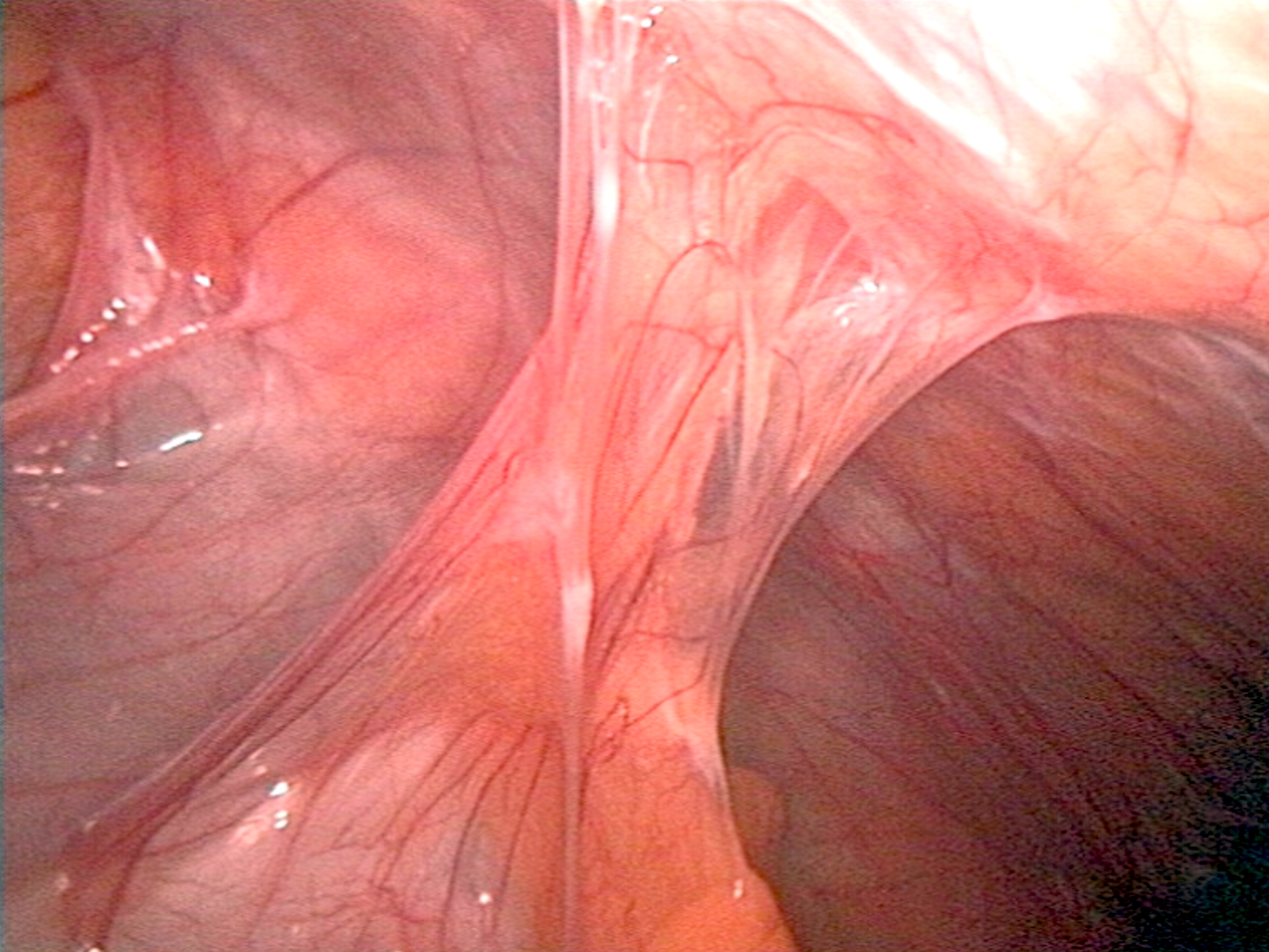
Image: Proud flesh

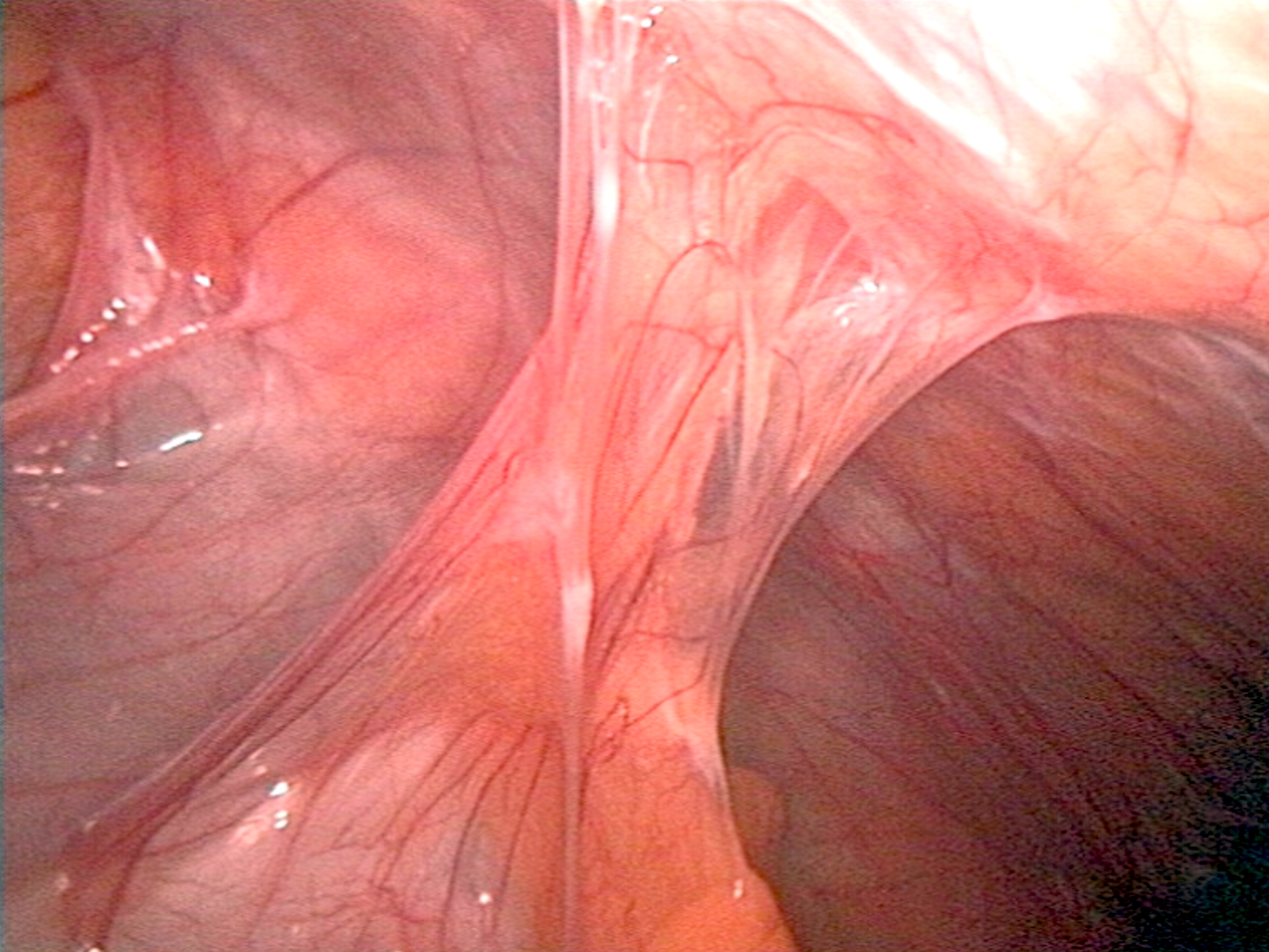
Thick dermal granulation tissue that results from an abnormal healing process.
Doctor could surgically cut back to the epithelial tissue level to reduce this type of scar tissues.
Image: Proud flesh

7.Hypertrophic scarring
"do not grow beyond the boundaries of the original wound"
Overgrowth of dermal tissue that remains within the boundaries of wound.
This scar is associated with deep partial or full thickness burns that have healed through second intension healing or with healing at the edges of skin grafts
8.Keloid
"spread into the surrounding normal skin. This results in chronic inflammation that may also explain the invasive growth of
keloids."
Scar tissue beyond the boundaries of original wound in a tumor-like growth.
Increased amount of collagen
Keloids do not respond well to surgical excision and they frequently recur.Corticosteroids are commonly used and more effective than surgery to reduce the scar.
Assessment
1.Observation
Edema?Pigmentation?
Raised?
Is it pulling the tissue surrounding?
Obvious limited ROM?
(Unable to extend the elbow fully as an example)
2.Palpation
Elasticity
Cold to touch? (Ischemia)
Loss of ROM
Loss of MSK tone
3.Testing
AROM
PROM
+
OP
Pain in the joint?
Significant limited ROM?
Any surrounding tissue pulled by ROM?
If yes, in which direction?
Weakness to the Overpressure?
Massage therapy
Hydrotherapy before the tx such as Paraffin wax are used with maturing scar tissue.
Rigid and restricted sections at the periphery of the scars are treated first to increase ROM
Tech: Skin rolling, S/C bowing, fascial spreading are used
Approach from least adhered to most adhered area
Go slow with client's pain tolerance over the series of tx
Always followed by passive stretch to promote alignment of the collagen fibres laid down during the healing process
Massage promotes the development of loose or areolar scar tissue rather than dense connective tissue scar
Post tx COLD hydrotherapy is appropriate after fractioning and any other tech where extreme hyperaemia and heat persist
"Basically, after moving the scar, you are promoting blood flow to the site which means more heat going there, so you could apply cold hydrotherapy to calm it down"
Get the idea??
Self care
So, what can they do at home?
Early stage of healing: Pain free ROM
Ranges are gradually increased as collagen matures through the late stage to chronic stage
Early subacute stage: Submaximal isometric contraction
Late subacute stage: Increasing force of contraction as a scar tissue matures and prolonged passive stretch works very well
Chronic stage: Isotonic exerciser important not only to maintain strength but to build strength in dthe injured or formerly immobilized muscles
Strengthening of the antagonist muscles will help prevent contracture from developing in the agonist.
example: if flexor surface of the forearm is affected in an injury, the extensors are strengthened to counteract the tendency of the wrist to be drawn into flexion as scar tissue contracts!
How frequent?
10 to 15 mins up to 6 times a day
7 days a week
Watch how the scar feels and start with a few times a day and increase the set as they could tolerate
7 days a week
Watch how the scar feels and start with a few times a day and increase the set as they could tolerate
Comments
Post a Comment